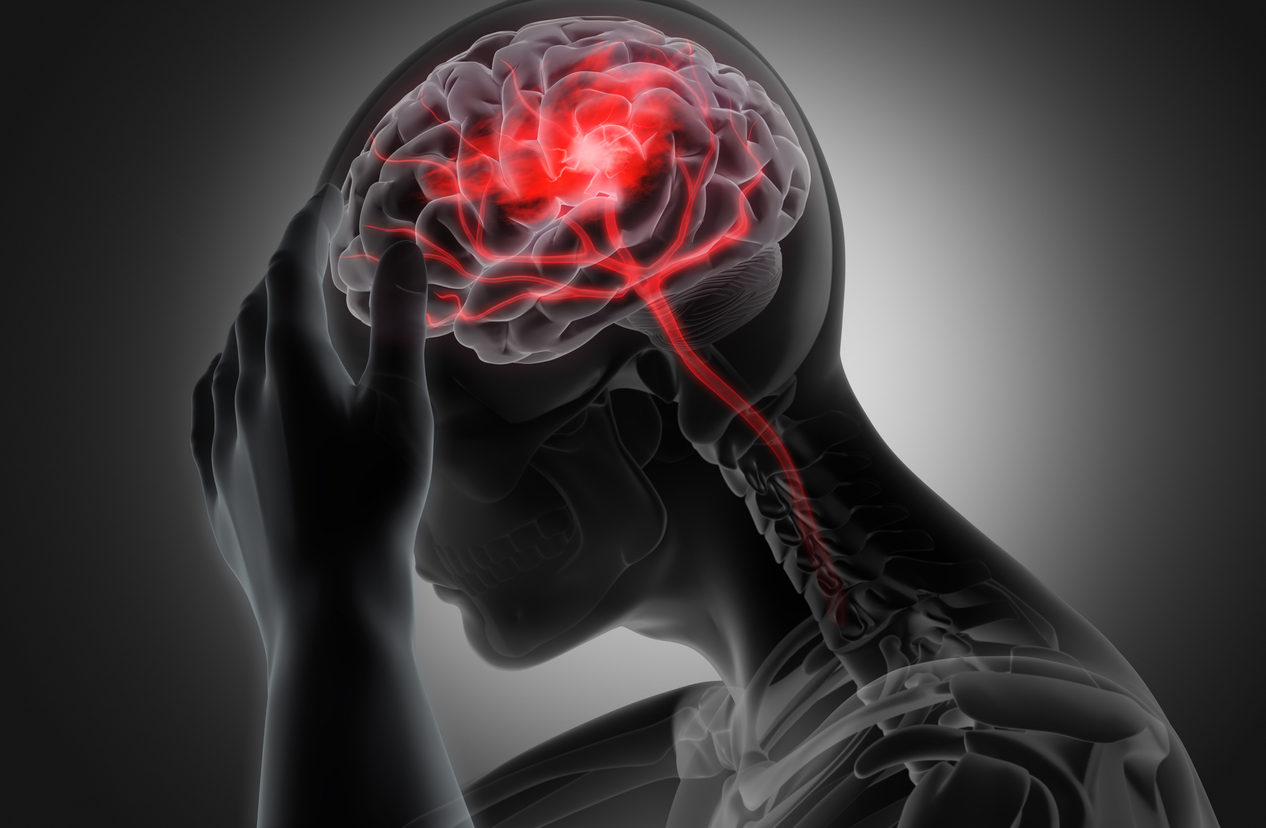
Pain
Tips for Supporting a Loved One With a Traumatic Brain Injury

What is a traumatic brain injury?
A traumatic brain injury (TBI) is a type of brain damage that occurs as a result of an injury to the head. This type of injury may be non-penetrative, such as a blow to the head, or penetrative, such as a gunshot wound. The severity of a TBI depends on various factors, and the lasting effects can range from a few days to permanent brain damage or, in severe cases, death. A concussion is the most common type of traumatic brain injury.
Don’t take their behavior personally
A TBI can cause changes in the brain that might alter behavior and personality. A person may say things they don’t mean, fail to understand sentences, take longer to process, become easily irritated, or have difficulty socializing. This can cause numerous communication issues. Try to understand that it is out of their control and not driven by intention.
Realize that they may need assistance
A person who has a TBI is likely to have difficulty with tasks that they were once able to complete easily. Interactions may become very different. Help may be needed with basic tasks, such as dressing, bathing, eating, etc.
Set boundaries
While a loved one may experience changes and require additional support, it is okay to set boundaries. Caregiver burnout can cause physical and emotional feelings of being unsafe. The caregiver must also set time to take care of themselves. The health and safety of both individuals are of utmost importance.
Understand that social abilities may be different
A person with a TBI may experience decreased sociability. They may tire easily, have difficulty understanding conversations or forming words, or be unable to parse certain verbal and nonverbal cues. Additionally, they may have problems with noises and bright lights. However, they still want to be included. Try to socialize with them when they are able and without rigid expectations. It may be beneficial to change the setting of social interactions. For instance, a loud and crowded bar may be overwhelming, but watching a movie at home or having a small cookout with only close family and friends may be rewarding.
Avoid infantilization
Your loved one is still there. Whenever possible, avoid speaking for them, making decisions for them, or speaking about them as if they are not there. Communications and reactions may take longer; however, it is important to allow them the ability to be their own person and have a sense of autonomy.
Be aware of triggers
Certain topics, people, sensory input, etc., may trigger an individual with a TBI to become agitated. They may become confused or experience certain symptoms, such as headaches. Be aware of how the environment impacts a loved one’s mood and physical or mental wellbeing in order to avoid triggers.
Communicate in a simple way
Those with a TBI may have difficulty with multistep processes, open-ended questions, sarcasm, arguments, and remembering details. When communicating with a loved one who has sustained a TBI, keep conversations simple. Avoid complex language, instructions with more than one or two steps, and countless details. Questions should be simple with yes or no answers. This makes conversations easier for them to understand.
Believe and validate
Oftentimes, a person with a TBI experiences emotional and physical difficulties. When these are expressed, listen to the individual and validate what they are feeling, even if it is not understood. Minimizing language should be avoided in response to a loved one’s pain. For example, avoid saying, “you are so lucky to even be alive.” If a loved one expresses suicidal ideation, take it seriously. It may be beneficial for them to seek counseling or talk to a medical professional.
Additional sources: Post Acute Medical Health and Cognitive FX