Pain
Diagnosing Osteoporosis
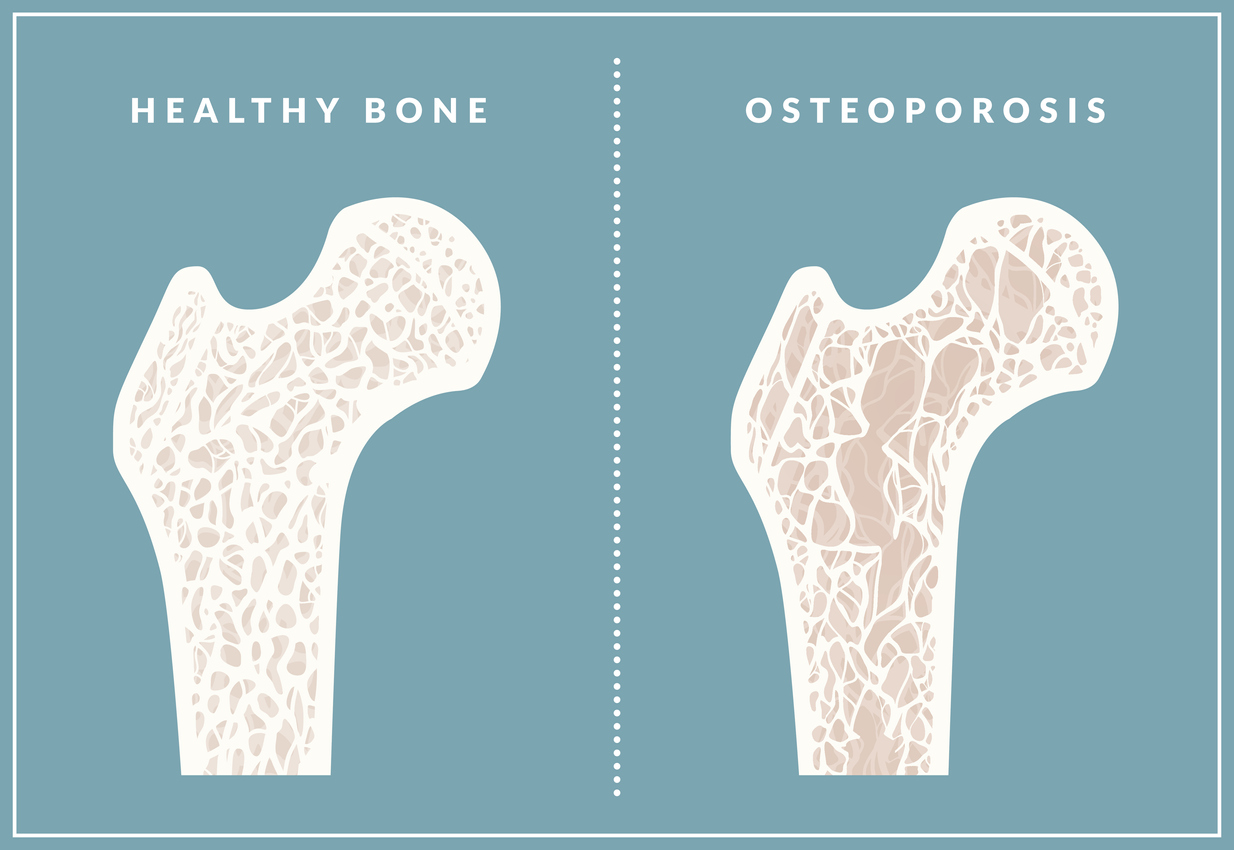
What is osteoporosis?
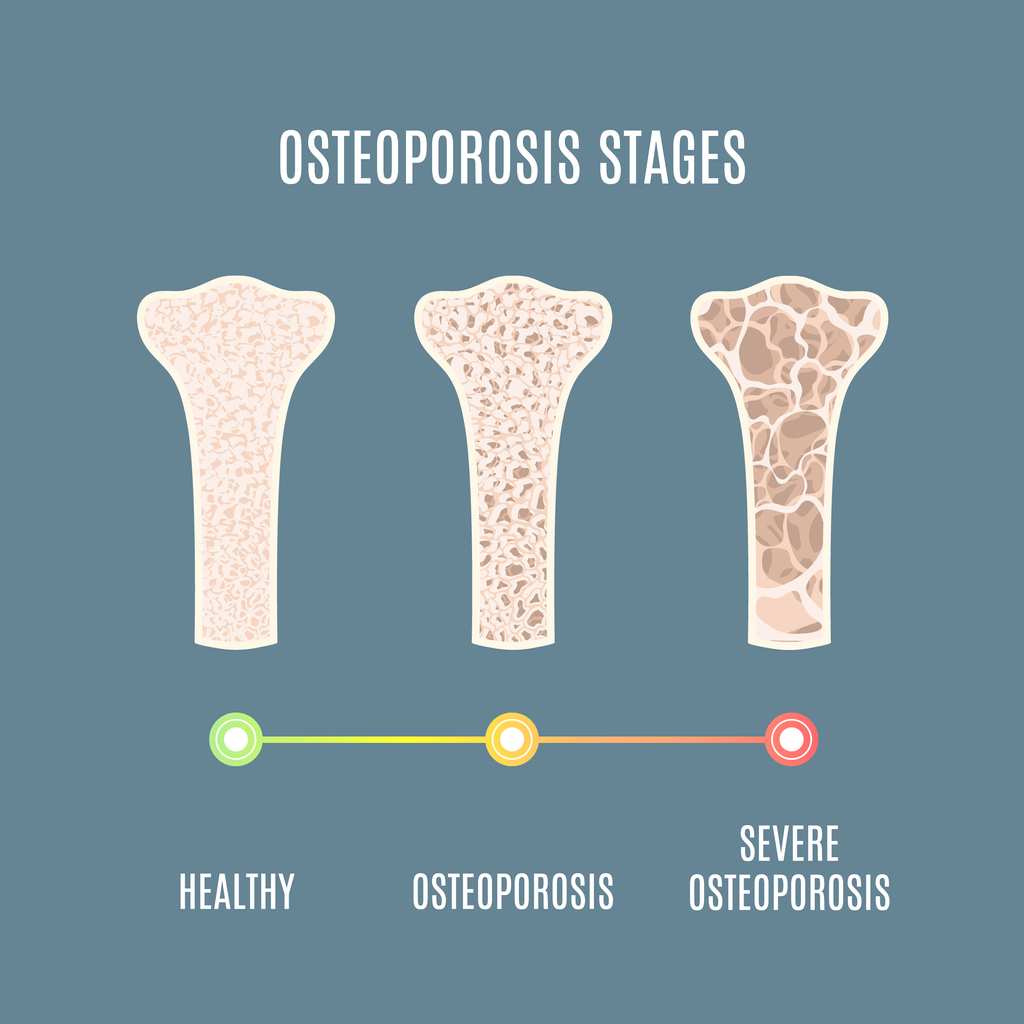
Osteoporosis is a condition that causes porous bones. The inside of a bone resembles a honeycomb. Osteoporosis causes this “honeycomb” spacing to increase, resulting in lost strength and density. The outside of the bones become brittle and weak.
This risk of fractures and breaks is increased with osteoporosis. An activity as simple as walking can cause a bone to fracture. In severe cases of osteoporosis, bones may become so brittle that a break can occur simply from coughing or bending the body. The bones most commonly affected by osteoporosis include the ribs, hips, wrists and spine.
Diagnosing osteoporosis
A health care professional will gather a medical history. This can include family history and lifestyle choices, such as physical activity, diet, and alcohol or tobacco use. A description of symptoms and frequency of symptoms will be evaluated. Current medications and medical conditions will be reviewed. A physical examination and certain testing will determine the diagnosis of osteoporosis.
Physical exam
A physical examination may involve measuring the height. Becoming shorter over time can indicate osteoporosis, as the bones of the spine are impacted. Individuals may also be asked to rise from a seated position without using their arms to push up.
Bone density scan
A dual-energy X-ray absorptiometry (DEXA), or bone density, scan measures the mineral content of the bones. Low levels of X-rays check bone density to determine how much bone loss has occurred.
Quantitative computed tomography
A quantitative computed tomography (QCT) also measures bone density. Radiation exposure with QCT is greater than other bone density testing. Accuracy also tends to be lower, although it still lies within the acceptable range.
Ultrasound
An ultrasound may be useful in detecting early signs of osteoporosis. The heel or other areas may be scanned with an ultrasound wand, which emits high-intensity sound waves. This allows for internal structure to be seen.
Blood and urine tests
Blood and urine tests can rule out other conditions that cause bone loss. They may also be ordered to determine which osteoporosis “markers” are present. Levels of proteins, enzymes, etc., can indicate the progression and provide other useful information. Calcium levels, thyroid function, and testosterone levels in men are provided. Bone-specific alkaline phosphatase and osteocalcin can indicate the rate of bone formation. Urinary N-telopeptide of type I collagen shows the rate of bone loss. Vitamin D levels may be tested, since they impact the absorption of calcium.
Additional source: ScienceDirect