Pain
Conventional Treatments for Spinal Stenosis

What is spinal stenosis?
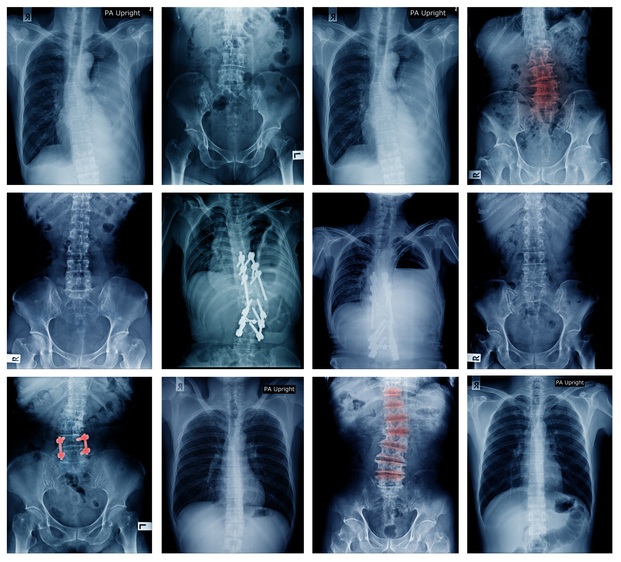
Spinal stenosis is a narrowing of the spinal canal. It occurs when the bony openings within the spine (foramina) begin to narrow, placing pressure on the nerves traveling throughout the spine. This reduced nerve space can occur within the spinal cord or where the spinal nerves exit the spinal canal. Spinal stenosis most commonly affects the upper neck (cervical) and lower back (lumbar); however, although rare, the upper and middle back (thoracic) can also be affected.
Treatments for spinal stenosis
The goals of treatment for spinal stenosis are to relieve pain and improve mobility and function. Several types of non-surgical treatments are available for spinal stenosis, including physical therapy, medications, and spinal injections.
Physical therapy
The goals of physical therapy for spinal stenosis are to strengthen the abdominal and back muscles, maintain flexibility of the spine, promote overall fitness, and improve balance. While physical therapy cannot cure spinal stenosis, it keeps the body active, preventing complications from inactivity.
Neck or back braces
A neck or back brace can prevent the spine from moving in a way that causes pain. However, wearing a brace can lead to weakening of the muscles, so braces should only be worn for short periods of time.
Medication options
Medications used to treat spinal stenosis include, but are not limited to, the following:
- Acetaminophen works on the central nervous system to relieve pain.
- Nonsteroidal anti-inflammatory drugs (NSAIDs) reduce inflammation and pain. Common NSAIDs include ibuprofen, naproxen, celecoxib and aspirin.
- Oral corticosteroids are powerful anti-inflammatory medications typically prescribed for severe back or leg pain.
- Anti-seizure medications reduce nerve-related pain, numbness, tingling or burning. Examples of anti-seizure medications include gabapentin and pregabalin.
- Tricyclic antidepressants can help ease chronic pain.
- Muscle relaxers are used to treat pain caused by muscle spasms.
- Opioid analgesics are prescribed for severe pain if other medications do not relieve pain.
Steroid injections
During an epidural or transforaminal spinal injection, a physician uses x-ray guidance and contrast dye to inject a long-acting steroid medication into the spaces around the compressed spinal nerves. A local anesthetic is injected before the steroid to help reduce procedure pain. Steroid injections work to decrease inflammation and reduce pain. This relief can last for weeks to months.
Minimally invasive surgery
- Interspinous process spacers
This procedure involves the implantation of devices between the bony protrusions at the back of the vertebra to increase space in the spinal canal. This procedure can often be performed with a local anesthetic. - Microendoscopic decompression
This form of decompression is done through a tube to minimize trauma to soft tissue and promote a faster recovery. Performing this type of surgery involves decreased visibility for the surgeon and is more difficult than traditional decompressions. It is not widely used. - Percutaneous image-guided lumbar decompression
Percutaneous image-guided lumbar decompression (PILD) is an option when dealing with lumbar spinal stenosis and a thickened ligament. In this procedure, a portion of the thickened ligament is removed using needle-like instruments; this increases space in the spinal canal, relieving pressure on the nerve roots. PILD is performed without general anesthesia, so it is not considered a surgical procedure.
Depending on individual symptoms and needs, a combination of treatments is typically used. If these conservative treatments do not work, surgery may be recommended.